In a previous post, we discussed the way the cilastatin prevents imipenem nephrotoxicity by inhibiting dihydropeptidase, a proximal tubular brush border enzyme which facilitates the uptake of imipenem metabolites into proximal tubular cells. This allows imipenem to be excreted unchanged in the urine. In the absence of cilastatin, imipenem would be unusable due to its significant adverse effects on the kidney.
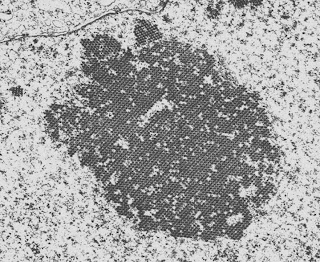
Approximately 40-60% of patients who receive cisplatin develop nephrotoxicity and this is its most common severe adverse effect. The mechanism of this nephrotoxicity is not entirely clear and has been discussed in the past by Emily and Nate. Primarily, however, it is due to proximal tubular cell damage with apoptosis of the affected cells leading to polyuria, a fanconi-type syndrome and ATN.
A paper was just published in KI which looked at the effect of co-administration of cisplatin and cilastatin in rats. The rats were given a single dose of cisplatin and those that received cilastatin had significantly less uptake of cisplatin into the renal cortex and lesser manifestations of renal toxicity. Interestingly, the uptake into the medulla was not affected and the half-life of cisplatin was longer than in the controls. Because dihydropeptidase is specific to the proximal tubule, it did not affect uptake into cancer cells and so anti-tumor activity was preserved. Cisplatin toxicity is the bane of the life of nephrologists working in major cancer centers because, once it has set in, there isn’t much that you can do and it limits the amount of treatment that these patients can get for their tumors. This is a preliminary study and we can’t say that this is the panacea for cisplatin nephrotoxicity but it certainly is promising as well as being a fascinating insight into the mechanisms of renal damage caused by cisplatin.